Bepreve
"Discount bepreve 5ml otc, symptoms blood clot leg."
By: William A. Weiss, MD, PhD
- Professor, Neurology UCSF Weill Institute for Neurosciences, University of California, San Francisco, San Francisco, CA

https://profiles.ucsf.edu/william.weiss
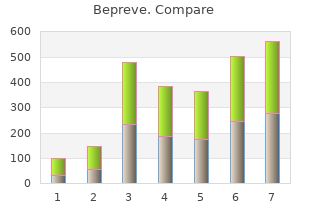
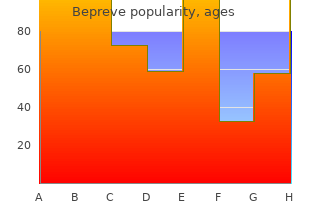
Clinical and pathological T/N stages were significantly different between all age groups (all p<0 generic bepreve 5 ml with mastercard. Tumor grade was significantly different between younger and older patients (all p<0 order bepreve 5 ml with amex. Notably cheap bepreve 5ml with visa, rates of de novo cM1 disease were comparable at the extremes of age (younger 3 generic bepreve 5 ml visa. Conclusions: Although significant differences in tumor biology and extent of treatment continue to exist between younger versus older breast cancer patients, the rarity of breast cancer in women over 75 years old was comparable to those under 45 years old. In a changing demographic of older women with breast cancer, thoughtful screening and treatment are important to prevent age-related disparities in breast cancer care. Inclusion criteria were female patients fi70 years old with Stage 1 3 invasive breast cancer. Results: There were 490 patients that met our criteria: 377 were clinical Stage 1A, 10 were Stage 1B, 64 were Stage 2A, 17 were Stage 2B, 14 were Stage 3A, 4 were Stage 3B, and 4 were Stage 3C. The secondary aim is to elucidate patient and treatment-related characteristics associated with high-volume centers. A Cox proportional hazards model with penalized cubic splines was used to examine the association between annual hospital volume and overall survival. High-volume centers were associated with a slightly younger patient population (84. Conclusions: Among elderly breast cancer patients age 80 or above, there is a significant association between undergoing surgery at a high-volume center (defined as fi270 cases/year) and improved survival. Patients in this population who undergo surgery at high-volume centers are characterized by an earlier stage of disease and more commonly receive breast-conserving surgery, as well as subsequent adjuvant radiation. We sought to identify clinical and histologic factors that predict upgrade to atypia or malignancy in a large population. Clinical, radiologic, and pathologic factors were compared in the no upgrade, upgrade to atypia, or upgrade to cancer groups. Univariate analysis was performed comparing no upgrade and upgrade to cancer or atypia. In the overall cohort, the presence of multiple papillomas in a single patient was a significant predictor of cancer or atypia (p=0. The clinical significance of identifying atypia in a papilloma is unknown, especially in a patient with a prior history of atypia. Roughly one-third of breastfeeding mothers indicated having insufficient milk production, of which 50% of these patients underwent prior surgery for fibroadenoma or macromastia. This multidisciplinary model can be adopted in programs looking for safe and effective ways to approach high-risk benign breast patients. We aimed to characterize the presentation and treatment of lactational phlegmon, a previously undescribed complication of mastitis that may require surgical management. Methods: We conducted a retrospective cohort analysis of women referred to a single breast surgeon for lactational mastitis between July 2016 and October 2018. Cases were categorized as uncomplicated mastitis, mastitis with phlegmon, or mastitis with abscess. Phlegmon was diagnosed by mass on physical exam with or without overlying erythema, as well as ultrasound demonstrating an ill-defined area of heterogeneous and hyperemic parenchyma, interdigitating fluid, and no discrete fluid collection. Aspiration was attempted in 7/10 phlegmon patients, with return of minimal non-purulent, serosanguinous fluid. Interval imaging was obtained in 2 patients due to persistent mass on follow-up exam, and both underwent core-needle biopsy for suspicious imaging findings, with pathology demonstrating acute and chronic mastitis. Aspiration does not appear to have an appreciable treatment effect, but an extended antibiotic course may reduce inflammatory and infectious symptomatology. We recommend follow-up examination and interval imaging to ensure complete resolution and to rule out occult mass as lead point for initial obstruction and inflammation. Breast surgeons are well-poised to manage lactational phlegmon as it may coalesce into an abscess requiring drainage and/or require biopsy in the setting of persistent mass. However, operating on adolescents remains controversial due, in part, to fear of potential postoperative breast regrowth. Results: A total of 564 subjects were included in analyses, with a mean age at surgery of 17. Although years since menarche was positively associated with macromastia severity, this association was no longer significant when examining healthy-weighted patients who were at least 2 years post menarche, and overweight/obese patients who were at least 7 years post menarche. Conclusions: Our findings suggest that maximum efficacy may be reached, and the risk for postoperative regrowth minimized, if reduction mammaplasty is performed at least 2 years post menarche in healthy weighted patients and at least 7 years post menarche in overweight/obese patients. The objective of this study was to determine the rate of upgrade to malignancy in patients with papilloma without atypia. Methods: A retrospective review of a prospectively maintained database of all cases of benign intraductal papilloma in a tertiary referral symptomatic breast unit was performed. Results: A total of 173 cases of benign papilloma diagnosed on core biopsy were identified, and 35 did not meet the inclusion criteria. Imaging on the day of planned surgery showed no residual corresponding 195 lesion in 2 patients. Conclusions: Patients with a diagnosis of benign papilloma with no atypia on core biopsy have a low risk of upgrade to malignancy on final pathology. However, further research is warranted to study the natural history of these lesions. In more recent series, the rate of upgrade of an intraductal papilloma without atypia (on core biopsy) to malignancy (on excision) is <10%. In order to inform the increasingly complex patient discussions around management of a papilloma without atypia diagnosed by core biopsy, it is important to examine our institutional upgrade rate from papilloma on needle core biopsy to atypia or malignancy on excisional biopsy. Any patient with the diagnosis of intraductal papilloma by core biopsy who underwent excision were included in the study.
Dual-energy role of Tc99m-sestamibi scintimammography in contrast-enhanced digital subtraction combination with the triple assessment of primary mammography: feasibility generic 5ml bepreve with mastercard. Case Analysis of intratumoral heterogeneity and report: complete lymphatic staging in breast cancer amplification status in breast carcinomas with by lymphoscintigraphy and sentinel node biopsy discount 5 ml bepreve otc. The stereotactic fine needle aspiration biopsy and role of magnetic resonance imaging in the stereotactic core needle biopsy in ductal carcinoma assessment of local recurrent breast carcinoma order bepreve 5ml. Relationship operative simultaneous stereotactic core biopsy and between long durations and different regimens of fine-needle aspiration biopsy in the diagnosis of hormone therapy and risk of breast cancer bepreve 5 ml line. Clonality analysis of quantization help to evaluate small mammographic intraductal proliferative lesions using the human lesionsfi Independent mannose-6-phosphate/insulin-like growth factor 2 validation of candidate breast cancer serum receptor coded by a breast cancer suppressor genefi Proc Natl Acad Sci U S A 2008 Nov 18; Not eligible target population 105(46):17937-42. Expression cyclooxygenase-2 expression in ductal carcinoma in of parathyroidlike protein in normal, proliferative, situ lesions and invasive breast cancer correlates to and neoplastic human breast tissues. Am J Pathol cyclooxygenase-2 expression in normal breast 1993 Oct; 143(4):1169-78. Pathology & Laboratory Medicine 2009 Jan; Percutaneous large-core biopsy of papillary breast 133(1):15-25. Atypical ductal hyperplasia diagnosed at stereotaxic Anticancer Res 1999 May-Jun; 19(3B):2275-9. Not core biopsy of breast lesions: an indication for eligible outcomes surgical biopsy. Can large trial experiences be Recurrent carcinoma after breast conservation: reproduced in a community hospital settingfi Not eligible target Percutaneous removal of malignant mammographic population lesions at stereotactic vacuum-assisted biopsy. Not eligible Calcification retrieval at stereotactic, 11-gauge, outcomes directional, vacuum-assisted breast biopsy. Not eligible needle biopsy of synchronous ipsilateral breast outcomes lesions: impact on treatment. One Epithelial displacement after stereotactic 11-gauge operation after percutaneous diagnosis of directional vacuum-assisted breast biopsy. Ann Surg Bracketing wires for preoperative breast needle Oncol 2009 Jan; 16(1):106-12. Correlation of mammographic appearance or to sample the mammographic target: what is the and molecular prognostic factors in high-grade goal of stereotactic 11-gauge vacuum-assisted breast carcinomas. Probably study of conservative surgery without radiation benign lesions at breast magnetic resonance therapy in select patients with Stage I breast cancer. Borderline eligible outcomes breast lesions diagnosed at core needle biopsy: can 1553. Aspects of early stages, progression and receptor downregulates E-cadherin gene expression related problems. Comparison age at first childbirth on risk of developing specific of loss heterozygosity in primary and recurrent histologic subtype of breast cancer. Flow Her-2/neu level predicts decreased response to cytometric and histological analysis of ductal hormone therapy in metastatic breast cancer. Cancer Res more likely than women from the United Kingdom 1982 Aug; 42(8 Suppl):3434s-6s. Breast improved prognosis for patients with T1N0M0 Cancer Res Treat 2008 Mar; 108(2):271-7. Cancer 2006 evaluation of residual disease in women receiving Nov 1; 107(9):2245-53. Role of reconstruction using the superior gluteus for free ultrasound and sonographically guided core biopsy tissue transfer: a case report. J La State Med Soc in the diagnostic evaluation of ductal carcinoma in 1988 Jun; 140(6):43-5. Tumori 2000 activation, normal T cell expressed and secreted Nov-Dec; 86(6):A13-8. Not eligible exemestane administered for 2 years versus placebo outcomes on bone mineral density, bone biomarkers, and 1614. Opportunistic patterns of allelic loss in estrogen receptor-positive breast cancer screening in Hong Kong; a revisit of infiltrating lobular and ductal breast cancer. Changes in incidence of reduction mammaplasty in reconstructing partial in situ and invasive breast cancer by histology type mastectomy defects. Megestrol Immediate endoscopic latissimus dorsi flap: risk or acetate versus aminoglutethimide for metastatic benefit in reconstructing partial mastectomy defects. N cytokeratin 7 expression is not restricted to Paget Engl J Med 1982 Oct 14; 307(16):1010-4. Not cells but is also seen in Toker cells and Merkel eligible target population cells. Experience with fine-wire localization breast Mammary gland anatomy and the role of biopsies for nonpalpable breast lesions detected mammography and ultrasonography in the early mammographically. The with breast cancer, cowden disease, and juvenile effectiveness of the Gail model in estimating risk polyposis.
Cheap 5 ml bepreve with mastercard. Qad Lamba karne ki Herbal Medicine | Apne Qad me izafa Kijiye.
A Cochrane review validated the perception that vaginal hysterectomy is the surgical route of choice for hysterectomy (42) order 5ml bepreve with amex. It compared abdominal hysterectomy with vaginal hysterectomy and three types of laparoscopic hysterectomies buy 5 ml bepreve with amex. The main observations were the shorter length of hospital stay cheap 5ml bepreve with amex, faster postoperative recovery cheap bepreve 5ml line, and decreased febrile morbidity of vaginal and laparoscopic hysterectomy compared with abdominal hysterectomy. The report concludes that there are improved outcomes with vaginal hysterectomy, and, when vaginal access is not possible, laparoscopic hysterectomy appears to have advantages over abdominal hysterectomy. Cost-analysis trials demonstrate that laparoscopic hysterectomy can be cost-effective relative to abdominal procedure but not compared with vaginal hysterectomy (43,44). The main cost determinants are the length of hospital stay and the use of disposable surgical devices. Risk of complication from each type of procedure provides insight into the proper options for the patient. The trial included conversion to laparotomy for the laparoscopic and vaginal groups as a major complication. If you include conversion to laparotomy as a major complication, the number treated relative to those harmed was 20 for the laparoscopic group compared with the abdominal group. If you exclude conversion to laparotomy as a complication, then the complication rates are similar between all groups. All six ureter injuries reported in this series occurred in the laparoscopic group. The overall lower urinary tract complication rate is three times higher with the laparoscopic group compared with vaginal or abdominal procedures. A minor complication, mostly postoperative fever or infection, occurred in approximately 25% of each group. Perioperative Checklist It is important to systematically go through a checklist of perioperative measures to effectively reduce potential complications (Table 24. If excessive blood loss is expected, intraoperative blood salvage techniques should be considered. All patients undergoing hysterectomy for benign disorders are at moderate risk for venous thromboembolism and require prophylaxis (18). Unfractionated heparin (5,000 U every 12 hours) or low molecular weight heparin. Patients on oral contraceptives up to the time of hysterectomy should be considered for pharmacologic treatment. Mechanical bowel preparation for prevention of infection complications from bowel injury is no longer recommended (46). Was the appropriate antibiotic selected according to American College of Obstetricians and Gynecologists guidelinesfi Document that prophylactic antibiotics will be discontinued within 24 hours after surgery. Technique Abdominal Hysterectomy General Preparation To reduce the colony count of skin bacteria, the patient is asked to shower. Hair surrounding the incision area may be removed at the time of surgery or before surgery using a depilatory agent. Hair clipping is preferable to shaving because it decreases the incidence of incisional infection, and if shaving is done, it should be performed in the operating room just prior to the surgery (34). Patient Positioning For most abdominal cases, the patient is placed in the dorsal supine position for the operation. After the patient is anesthetized adequately, her legs are placed in the stirrups and a pelvic examination is performed to validate the in-office pelvic examination findings. A Foley catheter is placed in the bladder, and the vagina is cleansed with an iodine solution. Skin Preparation Several methods for skin cleaning can be recommended, including a 5-minute iodine solution scrub followed by application of iodine solution, iodine solution scrub followed by alcohol with application of an iodine-impregnated occlusive drape, or an iodine-alcohol combination with or without application of an iodine-impregnated occlusive drape. Surgical Technique Incision the choice of incision should be determined by the following considerations: Simplicity of the incision Need for exposure Potential need for enlarging the incision Strength of the healed wound Cosmesis of the healed incision Location of previous surgical scars> the skin is opened with a scalpel, and the incision is carried down through the subcutaneous tissue and fascia. With traction applied to the lateral edges of the incision, the fascia is divided. This technique minimizes the possibility of inadvertent enterotomy, entering the abdominal cavity. Abdominal Exploration Cytologic sampling of the peritoneal cavity, if needed, should be performed before abdominal exploration. The liver, gallbladder, stomach, kidneys, para-aortic lymph nodes, and large and small bowel should be examined and palpated. Retractor Choice and Placement A variety of retractors were designed for pelvic surgery. The Bookwalter retractor has a variety of adjustable blades that can be helpful, particularly in obese patients. Elevation of the Uterus the uterus is elevated by placing broad ligament clamps at each cornu so that it crosses the round ligament. With the proximal portion held by the broad ligament clamp, the distal portion of the round ligament is ligated with a suture ligature or simply transected with Bovie cautery (Fig. The distal portion can be grasped with forceps, and the round ligament is cut to separate the anterior and posterior leaves of the broad ligament. The anterior leaf of the broad ligament is incised with Metzenbaum scissors or electrocautery along the vesicouterine fold, separating the peritoneal reflection of the bladder from the lower uterine segment (Fig.
It involves standardized counting and recording of sponges at the start of the case and as additional sponges are added to discount bepreve 5 ml amex the surgical field buy bepreve 5ml without a prescription. At the conclusion of the surgery cheap bepreve 5 ml amex, all sponges are placed in special transparent holders to generic 5 ml bepreve visa allow visual confirmation that all sponges were taken out of the patient. Other systems employ radiofrequency tagging of all sponges so that retained sponges can be detected easily before the surgical wound is closed (49). Clinical performance improvement: assessing the quality and safety of women�s health care. Some of the more sophisticated systems can check for errors and make suggestions based on preprogrammed guidelines and protocols. Avoiding abbreviations that may lead to medication error increases patient safety (51). Avoiding abbreviations that can be misread is an important and effective improvement, especially when orders are handwritten. One easily remembered and important rule about the written medication order is �always lead and never follow� a decimal point when using zeros. It can be very dangerous for the written period to be missed, resulting in 1 mg being given to a patient rather than 0. Bar coding of medications improves error occurrence by reducing the rate of wrong medication by nearly 75%. Other types of medication error improvements attributed to bar coding include incorrect dose, wrong patient errors, and wrong time errors, which were reduced substantially through the use of bar coding (52). Disruptive Provider Behavior In 2009, as part of its accreditation standards, the Joint Commission proposed that all health care organizations with professional staffs develop and implement a Code of Conduct Policy along with an education program that addresses disruptive behavior. Disruptive physician (provider) behaviors include inappropriate conduct in the hospital setting, resulting in conflict or confrontation. These behaviors can range from verbal and even physical abuse to sexual harassment. In recent years disruptive behavior in the hospital setting has become more evident, if not more common. One study showed that the vast majority of surveyed physicians, nurses, and administrators had witnessed disruptive behavior by physicians (53). Nurses and other hospital employees also commit disruptive behavior, but it is far less common than disruptive physician behavior. Having an accepted and agreed-upon verbal process to question or suggest changes in patient management improves communication. Team building that encourages collegial interaction and a sense that all members of the health care team are important and have something to offer can promote a culture that makes disruptive behavior less likely. Patient and Family Involvement in Quality and Safety One of the better definitions of quality is �meeting a customer�s (patient�s and their families) expectations. The Joint Commission, in collaboration with the Centers for Medicare and Medicaid Services, introduced an initiative they called �Speak Up. The program goal is designed to urge patients to take an active role in preventing health care errors by becoming involved and informed participants as members of the health care team. In 2008 a survey conducted by the Joint Commission indicated that campaigns like Speak Up add significant value to the accreditation process (54). Eighty percent of the more than1,900 organizations that responded rated the program as good or excellent. Studies show that greater patient (and family) involvement in health care decision making results in improved satisfaction and better outcomes (55). Patients and their families traditionally have low self-efficacy or confidence that they can understand and actively participate during their health care. Disclosure and Apology for Adverse Events Organized medicine is increasing its focus on the prevention of medical error. A controversial issue involving medical error is the need to promptly disclose and apologize for any medical errors that occur. In the past many, if not most, health care organizations focused on managing the medical legal risk of medical error. The conventional wisdom was that any disclosure and apology for error would lead to litigation and bigger payouts. The Joint Commission and other professional organizations require or endorse active disclosure to the patient when adverse events occur, including those caused by error (56). Three programs are worth noting in any discussion of disclosure and apology for medical error. First is the University of Michigan�s patient safety program, which addresses the need to disclose medical error in several publications (57). Important points are made about a patient�s rights concerning disclosure of medical error and that an apology for errors can be a productive benevolent gesture rather than an admission of fault. The authors point out several fallacies about disclosure, including that disclosing medical error always leads to litigation and that error always means negligence. Lucian Leape, one of the fathers of the modern patient safety movement, pointed out that a patient has an ethical right to full disclosure of medical error (58). Although an apology is not an ethical right, it is a therapeutic necessity, according to Leape. Several programs are under way to test the assertion that disclosure and apology can decrease the likelihood of litigation. The Sorry Works Coalition, which is a coalition of doctors, insurers, and patient advocates, urges the use of full disclosure and apology for medical errors (60). They point out that the current tort system has failed, resulting in higher and higher malpractice premiums without decreasing the rate of medical error. Demands for caps on malpractice awards and greater disciplinary measures for providers are largely ineffective. The Sorry Works Coalition advocates early disclosure with apology and financial settlements without litigation as the way forward in dealing with medical error.