Meclizine
"Order meclizine 25 mg with amex, medicine you can take during pregnancy."
By: Bertram G. Katzung MD, PhD
- Professor Emeritus, Department of Cellular & Molecular Pharmacology, University of California, San Francisco
http://cmp.ucsf.edu/faculty/bertram-katzung
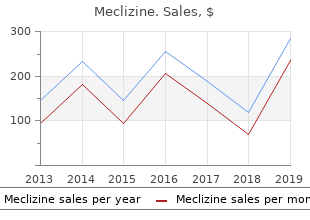
However meclizine 25 mg free shipping medicine that makes you throw up, 5% mannitol is strict monitoring of fluid deficit buy generic meclizine 25 mg line treatment 0 rapid linear progression, preferably with isosmolar and is an osomotic diuretic purchase meclizine 25 mg amex medicine journey, features that weighted monitoring systems and the adherence to insti- make it theoretically safer than other electrolyte-free tutionally predetermined fluid loss guidelines order meclizine 25mg line medicine quest. Provided adequate training, available equipment, and lower genital tract burns may be reduced by maintaining appropriate analgesia or anesthesia, small submucous contact of the external sheath with the cervix, avoiding myomas can be removed in the office setting. There may be a role for concomitant laparoscopy or is not in contact with tissue, ensuring the sustained in- ultrasound when hysteroscopic myomectomy is per- tegrity of the electrode insulation, and minimizing formed on deep type 2 submucous myomas. Intrauterine adhesions can be minimized if opposing tis- performing hysteroscopic submucous myomectomy. Second-look hysteroscopy may be effective for postop- mon after multiple submucous myomectomies. In such erative intrauterine adhesions and thereby could reduce circumstances, and when fertility is an issue, second- the long-term risk of adhesion formation. Recommendations for Future Research the Following Recommendations and Conclusions are 1. Prospectively evaluate of the impact of selective leio- otherwise classified) myoma ablation on submucous myomas, the molecular 1. Canadian Task Force on the Periodic profile of the adjacent endometrium and the related Health Examination. Long-term studies on the impact of various endometrial cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Comparative evaluation of the efficacy and effective- uterusandtheendometrium:lowprevalenceofleiomyomainarandom ness of different methods for preparation of the cervix sample of women age 25–40 years. Comparative evaluation of clinically relevant outcomes surveillance in the United States, 2000–2004. Estrogen and progesterone receptors in uterine leiomyo- sound and/or laparoscopy on the safety and efficacy of mas. Clinical signifi- resectoscopic myomectomy for type 2 leiomyomas cance of cytogenetic abnormalities in uterine myomas. Submucous and outer my- molecular characteristics of the endometrium and myo- ometrium leiomyomas are two distinct clinical entities. Further evaluation of the role of anti-adhesion agents resection of submucous fibroids for abnormal uterine bleeding: results after hysteroscopic myomectomy is of clinical impor- regarding the degree of intramural extension. J Minim Invasive Gyne- Practice Committee have reported the following financial col. Benign uterine disease: leiomyomata and coma in a series of hysterectomies performed for presumed uterine benign polyps. Miscellaneous uterine malignant neoplasms detected hysterosalpingography and hysteroscopy in the detection of intrauter- during hysteroscopic surgery. Diagnostic value of hyster- Diagnostic hysteroscopy in abnormal uterine bleeding: a systematic osalpingography in the detection of intrauterine abnormalities: review and meta-analysis. A systematic review of patient selection in 1202 patients with abnormal uterine bleeding. Fernandez H, Sefrioui O, Virelizier C, Gervaise A, Gomel V, magnetic resonance imaging. Magnetic resonance imaging and transvaginal ultrasonogra- atology, and management. Risk factors for uterine fibroids: reduced risk associated with oral A need for a debate? Prim Care mata in patients with a normal endometrial cavity on in vitro Update Obstet/Gynecol. International Committee for Contra- myomectomy on the outcome of assisted reproductive technologies. Submucous patterns in users of the levonorgestrel-releasing intrauterine system myomas and their implications in the pregnancy rates of patients with idiopathic menorrhagia or menorrhagia due to leiomyomas. Submucosal uterine leiomyomas have medroxyprogesterone acetate on surgically treated uterine leiomyo- a global effect on molecular determinants of endometrial receptivity. Mid- trozole) and gonadotropin-releasing hormone agonist (triptorelin) on term outcome of radiofrequency thermal ablation for symptomatic uterine leiomyoma volume and hormonal status. Aust agonist and iron versus placebo and iron in the anemic patient before N Z J Obstet Gynaecol. Directed laparoscopic cryomyol- ministration of tibolone plus gonadotropin-releasing hormone agonist ysis for symptomatic leiomyomata: one-year follow up. J Minim for the treatment of uterine leiomyomas: effectiveness and effects on Invasive Gynecol. Temporary uterine ar- focused ultrasound surgery for the treatment of uterine fibroids. Fertil tery occlusion for treatment of menorrhagia and uterine fibroids using Steril. Treatment of uterine myomas myomas: from six to twelve months after volume reduction. J Minim with transvaginal uterine artery occlusion: possibilities and limita- Invasive Gynecol. Cochrane Database Syst with abdominal hysterectomy for treatment of uterine leiomyomas. Guidance of focused ultra- embolization for treatment of leiomyomata: long-term outcomes sound therapy of uterine fibroids: early results. Complications after uterine artery embolization for leio- myoma-induced menorrhagia under local anesthesia. Treatment of Endometrial Ablation System in patients with intracavitary disease: uterine fibroids with implants of gonadotropin-releasing hormone ag- 12-month follow-up results of a prospective, single-arm clinical study. Short-term and long-term results management of menorrhagia in women with submucous myomas: of resectoscopic myomectomy with and without pretreatment with 12- to 20-month follow-up.
A stable plasma level of levonorgestrel of 150-200 pg/mL occurs after the first few weeks following insertion of Mirena generic meclizine 25mg without a prescription symptoms of pregnancy. Levonorgestrel levels after long-term use of 12 discount 25 mg meclizine mastercard medications 2015, 24 25 mg meclizine with mastercard medications xyzal, and 60 months were 180±66 pg/mL cheap meclizine 25mg on-line in treatment 1, 192±140 pg/mL, and 159±59 pg/mL, respectively. The plasma concentrations achieved by Mirena are lower than those seen with levonorgestrel contraceptive implants and with oral contraceptives. Unlike oral contraceptives, plasma levels with Mirena do not display peaks and troughs. The endometrial tissue concentration in 2 women who had been taking a 250 μg levonorgestrel–containing oral contraceptive for 7 days was 3. In contrast, fallopian tube and myometrial levonorgestrel tissue concentrations were of the same order of magnitude in the Mirena group and the oral contraceptive group (between 1 and 5 ng/g of wet weight of tissue). The pharmacokinetics of levonorgestrel itself have been extensively studied and reported in the literature. Levonorgestrel in serum is primarily bound to proteins (mainly sex hormone binding globulin) and is extensively metabolized to a large number of inactive metabolites. Metabolic clearance rates may differ among individuals by several fold, and this may account in part for wide individual variations in levonorgestrel concentrations seen in individuals using levonorgestrel–containing contraceptive products. The elimination half-life of levonorgestrel after daily oral doses is approximately 17 hours; both the parent drug and its metabolites are primarily excreted in the urine. Pharmacokinetic studies of this product have not been conducted in special populations (pediatric, renal insufficiency, hepatic insufficiency, and different ethnic groups). Drug-Drug Interactions the effect of other drugs on the efficacy of Mirena has not been studied. In study sites having verifiable data and informed consent, 1169 women 18 to 35 years of age at enrollment used Mirena for up to 5 years, for a total of 45,000 women- months of exposure. However, due to limitations of the available data a precise estimate of the pregnancy rate is not possible. Congenital or acquired uterine anomaly including fibroids if they distort the uterine cavity. Acute pelvic inflammatory disease or a history of pelvic inflammatory disease unless there has been a subsequent intrauterine pregnancy. Known or suspected uterine or cervical neoplasia or unresolved, abnormal Pap smear. Untreated acute cervicitis or vaginitis, including bacterial vaginosis or other lower genital tract infections until infection is controlled. Ectopic Pregnancy Evaluate women who become pregnant while using Mirena for ectopic pregnancy. The incidence of ectopic pregnancy in clinical trials that excluded women with risk factors for ectopic pregnancy was about 1 ectopic pregnancy per 1000 users per year. Tell women who choose Mirena about the risks of ectopic pregnancy, including the loss of fertility. Teach them to recognize and report to their physician promptly any symptoms of ectopic pregnancy. Women with a previous history of ectopic pregnancy, tubal surgery or pelvic infection carry a higher risk of ectopic pregnancy. The risk of ectopic pregnancy in women who have a history of ectopic pregnancy and use Mirena is unknown. Intrauterine Pregnancy If pregnancy should occur with Mirena in place, Mirena should be removed. Continuation of pregnancy If a woman becomes pregnant with Mirena in place and if Mirena cannot be removed or the woman chooses not to have it removed, she should be warned that failure to remove Mirena increases the risk of miscarriage, sepsis, premature labor and premature delivery. She should be followed closely and advised to report immediately any flu-like symptoms, fever, chills, cramping, pain, bleeding, vaginal discharge or leakage of fluid. Long-term effects and congenital anomalies When pregnancy continues with Mirena in place, long-term effects on the offspring are unknown. Because of the intrauterine administration of levonorgestrel and local exposure of the fetus to the hormone, the possibility of teratogenicity following exposure to Mirena cannot be completely excluded. Some observational data support a small increased risk of masculinization of the external genitalia of the female fetus following exposure to progestins at doses greater than those currently used for oral contraception. In some cases, severe pain occurred within hours of insertion followed by sepsis within days. Patients must be taught to recognize and report to their physician promptly any symptoms of pelvic inflammatory disease. These symptoms include development of menstrual disorders (prolonged or heavy bleeding), unusual vaginal discharge, abdominal or pelvic pain or tenderness, dyspareunia, chills, and fever. Irregular Bleeding and Amenorrhea Mirena can alter the bleeding pattern and result in spotting, irregular bleeding, heavy bleeding, oligomenorrhea and amenorrhea. During the first three to six months of Mirena use, the number of bleeding and spotting days may be increased and bleeding patterns may be irregular. Thereafter the number of bleeding and spotting days usually decreases but bleeding may remain irregular. If bleeding irregularities develop during prolonged treatment, appropriate diagnostic measures should be taken to rule out endometrial pathology. The possibility of pregnancy should be considered if menstruation does not occur within six weeks of the onset of previous menstruation.
If this is not available buy discount meclizine 25mg online medications covered by medicare, use a non stretchable tape measure attached to a vertical buy meclizine 25 mg visa symptoms bone cancer, fat surface like a wall or a door jam with no baseboard and equipment that will provide an accurate right angle to actually take the measurement meclizine 25 mg discount medications you can give your cat. The movable measuring rod that is attached to a platform scale is too unsteady to ensure accurate measurements generic 25mg meclizine fast delivery abro oil treatment. Technique for Height Measurement (3,4) Two people may be required for accurate measures of younger children, however, usually only one measurer is required for Figure 5. Measure the child with underclothes only, if possible, or with non-bulky clothing and no shoes. Have the child stand with heels together and touching the foor, knees straight, arms at sides, shoulders relaxed, and shoulder blades, buttocks, and heels touching the wall or measuring surface. Have the child look straight ahead with her line of vision perpendicular to the body. Technique for Stature Estimation: Sitting Height Use the same equipment as that described for measuring standing height, except have the child sit on a box of known height and subtract the height of the box from the measurement obtained. Sitting height should not be measured with the child sitting on the foor or on a box with legs extended outward in a 90˚ angle (3). Technique for Stature Estimation: Arm Span (7) Arm span is defned as the greatest distance between the tips of the extended middle Figure 6. Measuring Sitting Height fngers of the right and left hands when the arms are fully extended to the sides at right angles to the body and the back is straight. Measurement of the arm span is useful for estimating the stature of persons with lower extremity contractures or lower body Nutrition Interventions for Children With Special Health Care Needs 19 Chapter 2 - Anthropometricss paralysis. For the typically developing child over age six, the ratio of arm span to height has been found to be 1:1. This may not be the case for the child with special health care needs; however, monitoring an individual’s arm span measurements over time can provide some information about growth. Arm span is not an adequate substitute for stature in persons with contractures of the upper extremities (e. Also, arm span cannot accurately estimate stature in young children (younger than 5 to 6 years) because the proportions of limb length and trunk length to total body length are different for younger than older children. Equipment for Arm Span Measurement Arm span measurements are made with an anthropometer, a stainless steel detachable rod approximately seven feet long with etched gradations to 0. Technique for Arm Span Measurement Two people are needed to measure arm span Person A 1. Hold the fxed end of the anthropometer at the tip of the middle fnger of one of the child’s hands. Position the sleeve at the tip of the middle fnger of the child’s other hand with the anthropometer going across the child’s back. Have the child stretch her arms while the movable sleeve is adjusted to the maximum arm span. Record the actual numeric value, and plot as height for age on the appropriate growth chart. Weight Infants and toddlers less than 12 kg or 25 lbs can be accurately weighed on an infant scale. An accurate measure of weight is critical—it is more valuable to obtain an accurate bi-annual weight than a series of inaccurate monthly weights. Equipment for Weight Measurement Use a calibrated beam balance scale with non-detachable weights or a digital scale with a “strain-gauge” mechanism. To weigh infants and young children who cannot stand, use a pan-type or bucket seat-type pediatric scale that is accurate to within 0. For older children who can stand, use a platform beam scale, or an electronic scale that is accurate to within 0. Do not use a spring type bathroom scale which, with repeated use, will not maintain the necessary degree of accuracy. For children who are too large for the infant scale, but cannot stand, use a platform scale on which a wheelchair can be placed, or a bed scale. Since this type of specialty scale is not available in many communities, it can be diffcult to regularly monitor the weight of children with special health care needs. An alternative is to weigh the child’s caregiver holding the child, weigh the caregiver alone, and subtract the caregiver’s weight from the weight of both individuals. Frequently check and adjust the zero weight on the beam scale by placing the main and fractional sliding weights at their respective zeros and moving the zeroing weight until the beam balances at zero. If a pad or diaper is used to make the pan more comfortable, place it in the pan before the zero adjustment is made; otherwise, the weight of the pad or diaper must be subtracted from the weight of the child each Figure 8. Scales Nutrition Interventions for Children With Special Health Care Needs 21 Chapter 2 - Anthropometricss time a measurement is made. At least two or three times per year have the accuracy of the scale checked with a set of standard weights by a local dealer or an inspector of weights and measures. Record the numeric value and plot weight for age and weight for length on the appropriate growth chart(s). Record any information about conditions that might have interfered with an accurate weight measure (e. Weigh the child with only lightweight undergarments or a hospital gown and no shoes. Have the child stand in the center of the scale’s platform touching nothing and with heels together. Record the numeric value and plot weight for age and weight for height on the appropriate growth chart(s). Record any information about conditions that might have interfered with an accurate weight measure (e. There are separate charts for girls and boys ages 0 to 36 months; they include weight for age, recumbent length for age, and weight for length. These charts are most useful if measurements are accurately obtained and plotted on a regular basis so that the child’s growth pattern can be observed.
Several studies have compared shorter (3 or 5 days) and longer diary durations (7 days) [23-28] generic 25mg meclizine amex symptoms 4dp3dt. Two studies have demonstrated the reproducibility of voiding diaries in both men and women [23 buy meclizine 25 mg with visa 97140 treatment code, 28] buy meclizine 25mg fast delivery symptoms 8dp5dt. Further studies have demonstrated variability of diary data within a 24-hour period and compared voided volumes recorded in diaries with those recorded on uroflowmetry [29 purchase 25mg meclizine overnight delivery medicine to reduce swelling, 30]. Other studies have investigated the correlation between data obtained from voiding diaries and standard symptom evaluation [31-34]. A* If a symptomatic urinary tract infection is present with urinary incontinence, reassess the patient after A* treatment. Do not routinely treat asymptomatic bacteriuria in elderly patients to improve urinary incontinence. It indicates poor voiding efficiency, which may result from a number of contributing factors. A Measure post-voiding residual in patients with urinary incontinence who have voiding symptoms. B Measure post-voiding residual when assessing patients with complicated urinary incontinence. C Post-voiding residual should be monitored in patients receiving treatments that may cause or worsen B voiding dysfunction. These Guidelines will focus on invasive tests, including multichannel cystometry, ambulatory monitoring and video-urodynamics, and different tests of urethral function, such as urethral pressure profilometry, Valsalva leak point pressure estimation and retrograde urethral resistance measurement. Numerous small studies of multichannel cystometry have been done over many years in differing populations. Whilst in healthy women the same session repeatability has been shown to be poor [51], in those with incontinence it may be acceptable [52]. Abdominal or Valsalva leak point pressures may correlate to incontinence severity [57] but the tests are not standardised and there is no evidence about reproducibility. The problem is that clinical diagnosis and urodynamic findings often do not correlate [58, 59], and normal healthy people may have urodynamic abnormalities. The diagnostic accuracy of urethral pressure profilmetry [53] and ‘Urethral Retro resistance’ is generally poor [60]. Urethral reflectometry may have greater diagnostic accuracy but its clinical role remains unclear [61]. Ambulatory urodynamics may detect unexpected physiological variance from normal more often than conventional cystometry, but the clinical relevance of this is uncertain [62, 63]. Does urodynamics influence the outcome of surgery for stress urinary incontinence? Another similar study was closed with only 59 women [70] after finding no difference in outcome. It was then redesigned to randomise only women (N=109) in whom urodynamic findings were contradictory, to immediate surgery or treatment tailored to urodynamic findings. In this trial, performing immediate surgery irrespective of the result of urodynamics did not result in inferior outcomes [71]. Whilst low pre-operative flow rate has been shown to correlate with post operative voiding dysfucntion [74, 75], post hoc analysis of two high quality surgical trials showed that no pre-operative urodynamic parameter had the ability to predict post operative voiding dysfunction [76, 77]. Whilst urodynamics will distinguish causes of incontinence, its ability to predict outcome of surgery for incontinence for these men is uncertain [78, 79]. There is no evidence that urodynamics predicts the outcomes of treatment for post prostatectomy 4 incontinence in men. Advise patients that the results of urodynamics may be useful in discussing treatment options, C although there is limited evidence that performing urodynamics will predict the outcome of treatment for urinary incontinence. Do not routinely carry out urodynamics when offering conservative treatment for urinary incontinence. B Perform urodynamics if the findings may change the choice of invasive treatment. B Do not use urethral pressure profilometry or leak point pressure to grade severity of incontinence or C predict the outcome of treatment. A 1-hour pad test using a standardised exercise protocol and a diagnostic threshold of 1. Pad test with a specific short graded exercise protocol also has diagnostic value but a negative test should be repeated or the degree of provocation increased [84]. The usefulness of pad tests in quantifying severity and predicting outcome of treatment is uncertain [81, 85] although early post-operative testing may predict future continence in men after prostatectomy [86]. C Use repeat pad test after treatment if an objective outcome measure is required. One study suggested that mid-urethral sling placement decreased mobility of the mid-urethra but not mobility of the bladder neck [92]. Several imaging studies have investigated the relationship between sphincter volume and function in women [94] and between sphincter volume and surgery outcome in men and women [95, 96]. They are often used in combination which makes it difficult to determine which components are effective. Containment devices play an important role, especially for individuals who prefer to avoid the risks of interventional treatments, or in whom active treatment is impossible for any reason. These conditions include: • cardiac failure [103] • chronic renal failure • diabetes [103, 104] • chronic obstructive pulmonary disease [105] • neurological disease including stroke and multiple sclerosis • general cognitive impairment • sleep disturbances,. It is possible that correction of the underlying disease may reduce the severity of urinary symptoms. However, this is often difficult to assess as patients often suffer from more than one condition. There is also a risk that stopping or altering medication may result in more harm than benefit.
Purchase meclizine 25 mg amex. Odia Super Hits Dj Songs Full Remix 2017 New Year Special HINDI ODIA HD.